Anyone with internet access these days has their eyes on two constellations of data – the spread of the coronavirus, and the resulting collapse of the financial markets. Following the 13% one-day drop of the stock market a week ago, The Wall Street Journal forecast a quarterly GDP drop of as much as 10% – more than the worst quarter in the 2008 great recession. A coronavirus-induced recession will reinforce the health damage from the virus itself — one study of at-risk mothers found that the increased unemployment during the 2008 recession reduced the odds of having “excellent” or “very good” health status by 75% and increased the odds of smoking and using drugs, or of having serious mental health problems by more than 100%.
As serious as the actual health effects of the coronavirus have been, there have been fewer deaths, so far, than the annual flu average. What has shattered markets has been the uncertainty and fear of what is to come – the potential scope and mortality from coronavirus seem huge.
The comparison to the flu is relevant. If the coronavirus ultimately turns out to have a mortality rate similar to a severe flu, the most draconian restrictions can be relaxed sooner and economic life can resume. Published death rates for the main hot spots, China, Italy and Iran, range from 4% to 8% — frightening numbers given the rapid growth of the virus. There is a lot of uncertainty in these estimates, however, since there is limited information on how widespread the virus is – the all-important denominator in the calculation of a mortality rate. Let’s unpack two important rates: the rate of infection, and the rate of death among those infected.
The Rate of Infection
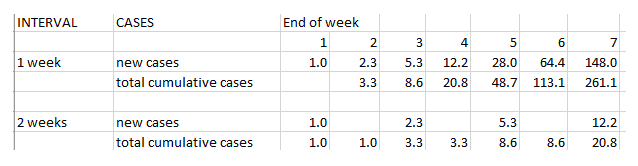
A key number in measuring the spread of a disease is its reproduction rate – how many additional people are infected by a new case. A related number is the interval time – the time between one case and the next. These two numbers determine the scope and speed of an infection. It is useful to explore the ramifications of these numbers – here’s an example with one initial case, an interval of 1 week, and a reproduction rate of 2.3 (the interval and rate used in this Annals of Internal Medicine article):
With an interval of 1 week, there are 261 cases at the end of seven weeks. If, through intervention, the transmission interval can be extended to 2 weeks, the number of cases at the end of the period drops to 21. It takes another six weeks before 261 is reached. This is a simple example that illustrates both the potency of exponential growth and the dramatic effect that countermeasures can have. Extending the transmission interval will also probably have the effect of reducing the reproduction rate, which calculation is not shown here. Extending the transmission interval beyond the period of contagiousness, and the reproduction rate drops to zero.
The reproduction rate for the flu is much less than the reported reproduction rate for coronavirus – for the flu, it is estimated variously at 1.3 and 1.5.
Mortality and the Denominator
Dr. Anthony Fauci, Director of the National Institute of Allergy and Infectious Diseases, has estimated the death rate from coronavirus at about 1%. This is roughly ten times as deadly as the flu, whose death rate is estimated at 0.1%, but much less than in hotbed countries, where death rates exceed 4%.
A rate, necessarily, is a numerator and a denominator. The numerator is pretty clear – there is hard data on the number of coronavirus deaths. But what about the denominator? Official calculations are based on a denominator that is the number of confirmed cases. Coronavirus symptoms are similar to the flu, so the only way to confirm a person has coronavirus is by laboratory testing. Two factors make the official denominator almost certainly an under-estimate:
- Many people have mild symptoms, and do not necessarily even seek treatment or testing
- A shortage of tests in many countries further restricts the denominator
But how much of an under-estimate?
Denominator for the Flu
At first, it might appear that the same considerations apply to the denominator for calculating the flu rate. However, more information is known about the flu, and officials do not rely solely on confirmed tested cases. The CDC also collects surveillance data on flu-like symptoms reported in out-patient visits, and by hospitals. Their methodology, honed over many years of experience, is described here. The Centers for Disease Control (CDC) estimates that there were approximately 35 million cases of the flu and 34,000 deaths in the U.S. during the 2018 – 2019 flu season (a death rate of just under 0.1%).
Denominator for Coronavirus
World Health Organization data on the coronavirus, as reported here, show 190,000 coronavirus cases, and 7500 deaths, for a death rate of 4%. Smaller numbers, overall, than the flu, but a much higher death rate. While the number of deaths is reported with some precision, the number of cases is certainly an under-estimate (see above). Let’s consider a couple of situations that offer a more controlled scenario.
Diamond Princess Cruise Ship
The Diamond Princess was placed in quarantine on Feb. 2, 2020 off Yokohama, Japan, after passengers were diagnosed with coronavirus. Out of 3711 passengers, virtually all were tested, and 619 (17.7%) ultimately became ill with coronavirus. 7 (1.1%) since died.
This offers a controlled laboratory of sorts, with a closed, fully tested population. It differs from real-world conditions in a couple of respects (the close quarters on the ship might hasten the spread of infection, while the early recognition of the danger led to rapid counter-measures). Nonetheless, it provides a good base-case scenario, and suggests that the infection rate in a closed system might be brought down to below 20%, and the death rate to about 1% (Dr. Fauci’s rate). If applied to the U.S., this would imply total infections of 60 million (almost double the flu), and deaths of 600,000 (10-20 times the flu).
However, the age profile of the Diamond Princess passengers is not that of most countries. Passengers 70 years old and older constituted a third of the passengers, but 46.5% of the illnesses and all 7 deaths. One research team took the illness and age profile of the Diamond Princess and applied it to China, making statistical adjustments, to come up with an “age adjusted mortality” estimate for China of 0.5%. This is half the crude mortality estimate, and the study is worth reviewing. However, the meager sample of 7 deaths is a thin reed upon which to build a complex statistical edifice and apply it to 1.4 billion people.
South Korea
South Korea is another instructive case. It has had a widespread testing program since the beginning of the crisis, 242,000 tested as of March 13, a higher rate than almost* any other country. As a result, a larger proportion of the actual cases in South Korea is identified (the denominator), so the published death rate (just under 1%) is probably closer to the long-run true rate.
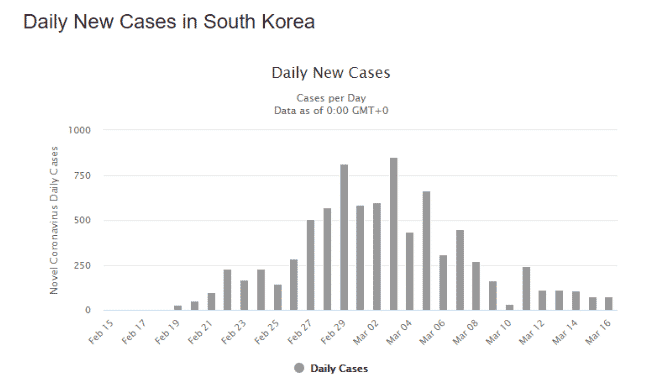
South Korea’s experience with MERS left its public health infrastructure better equipped to deal with a pandemic. The testing program itself is also credited with helping to limit the spread of coronavirus. Widespread testing is crucial to identifying individuals who are contagious, and can know to self-isolate. But if they are so identified, will they self-isolate? This depends on the strength of civic and community bonds, the degree of public information, and the confidence in that information. South Korean authorities have been open and transparent with information, and the national culture encourages social harmony and deference to authority. The result is a grass-roots driven policy and practice of voluntary social distancing. The effect is telling – the number of new covid-19 cases has dropped precipitously this month (source https://www.worldometers.info/coronavirus/country/south-korea/ ):
The better information afforded by widespread testing can also help mitigate the economic impact of the virus. With greater knowledge about who is infected and who is not, social distancing and quarantine can be better targeted and normal activity need not be so heavily impacted by massive blanket measures.
*Bahrain, with close population ties to Iran, a hotbed for coronavirus, has the most aggressive testing program in the world, but too few deaths to be statistically useful.
Conclusion on the Death Rate
With additional information on the denominator, 1% — ten times the flu death rate, but less than the worst hotbeds — seems a reasonable estimate for the coronavirus death rate in countries that implement effective and prompt countermeasures.
Testing in the United States
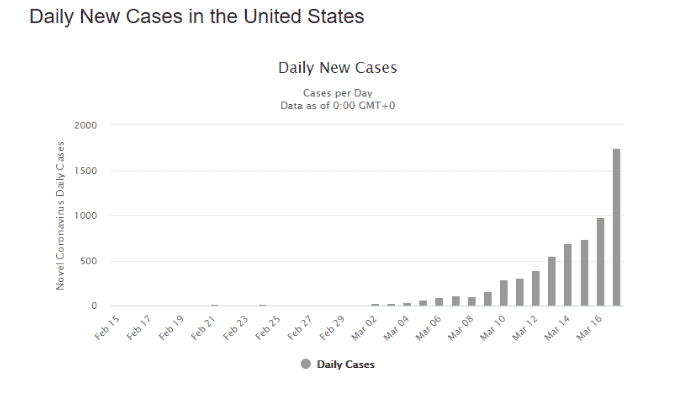
The U.S. is way behind in the testing arena, so may not be as fortunate as South Korea in quickly “flattening the curve.” The first coronavirus case was discovered in the U.S. and South Korea at about the same time, but while South Korea has completed over 5000 tests per million people, the U.S. has done less than 126 per million. And the U.S. is still on the steep upward path of growth:
Amazingly, the U.S. lacks a single reliable source on its testing efforts – the CDC has been reporting specimens tested, not people, states report separately, and an internet community-based effort, Covid-19 tracking, provides another data source for people tested. Production of tests should gear up with the approval that Roche received to begin making and distributing tests. Moreover, the U.S. government has not fully embraced the widespread testing philosophy that was key to controlling the virus in South Korea. In his March 13 press conference, President Trump said “…we don’t want people to take a test if — if we feel that they shouldn’t be doing it. And we don’t want everyone running out and taking — only … if you have certain symptoms.” As of today, the promised web site to direct potential virus victims to testing centers is still in its infancy, but Roche says it will start shipping 400,000 test kits this week.
With a large, borderless expanse, freedom of movement and a huge open economy, the United States is poorly situated to enforce strict quarantines and travel restrictions. Better and more readily available testing would allow more targeted mitigation and, together with credible and reliable information from the government, facilitate better-informed voluntary social distancing. This will hurt the economy less, which in itself could save lives and health.